What is vascular Ehlers-Danlos syndrome?
What is Ehlers-Danlos syndrome?
It is a syndrome with three symptoms: skin hyperextension (abnormally stretched when pinched), joint hypermobility, and connective tissue fragility (tissue tears or swells quickly).
It is caused by a genetic abnormality mainly related to collagen. There are 13 types, one of which is the vascular type (There is an explanation at the bottom of the page).
Impact of vascular Ehlers-Danlos syndrome
Vascular Ehlers-Danlos syndrome (EDS) is the most life-threatening type. Most of the patients sent for vascular surgery are urgent cases, such as aortic dissection, aortic aneurysm rupture, and vascular tear. In many cases, the diagnosis is not made at the time of admission. However, we consider vascular EDS as one of the differential diagnoses when we observe a young patient with arterial deterioration without arteriosclerosis. Other diagnoses include genetic diseases such as Marfan syndrome and other inflammatory diseases such as Behcet’s disease and Takayasu’s disease. Honestly speaking, we are scared to operate such a case because we frequently found that the tissues were very fragile, the suture lines collapsed sequentially, and blood vessels were easily obstructed by clots.
Cases of vascular EDS
There is a symbolic case of vascular EDS that has been handed down in our department. The patient underwent surgery for a ruptured SAA. We herein present a case of vascular EDS that had been treated in our department. Professor Miyata, a former professor at our department, and Professor Makuuchi, a former professor of hepato-biliary-pancreatic surgery, performed distal pancreatectomy and splenectomy. They said that it was very difficult to stop bleeding from the tissues they touched even if they sutured them with the needle repeatedly. Finally, they managed to stop major bleeding and saved his life with a large amount of blood transfusion. Therefore, the lesson from the case was that we should avoid open surgery as much as possible for cases of vascular EDS.
We have experienced many traumatic cases that demonstrated fragility of abnormal tissues including blood vessels, such as a case in which the iliac artery was completely torn and separated, and a case where the artery in the arm was suddenly torn during taping of the vessel during arteriovenous fistula creation.
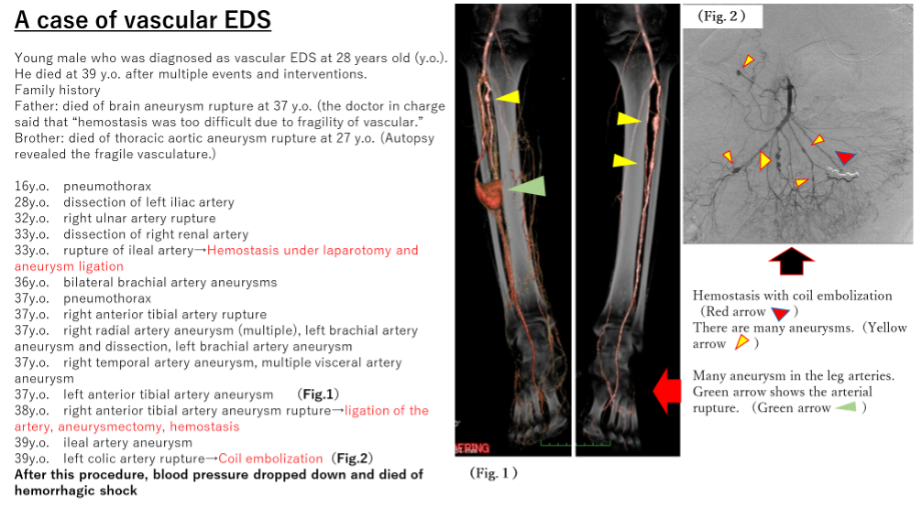
Please see the next case shown below (Fig. 1).
There was a lot of information in the past history and family history, which indicated vascular fragility. The red fonts indicate surgery performed in our department. Unfortunately, the patient died of hemorrhagic shock. However, we have learned a lot from this patient.
Lessons learned and our policies
Is “operation” for vascular EDS contraindicated? Currently, endovascular treatment (using catheters and wires, stents, and coils) is a tool, and I think that it should be given much priority over open surgery. However, open surgery should be performed for cases of gastrointestinal tract or uterus ruptures, or with massive hematoma due to vascular rupture. When developing a surgical plan, we have to consider how to approach the collapsed part, how to lessen the invasion of surgery, the patient’s background, and the postoperative quality of life.
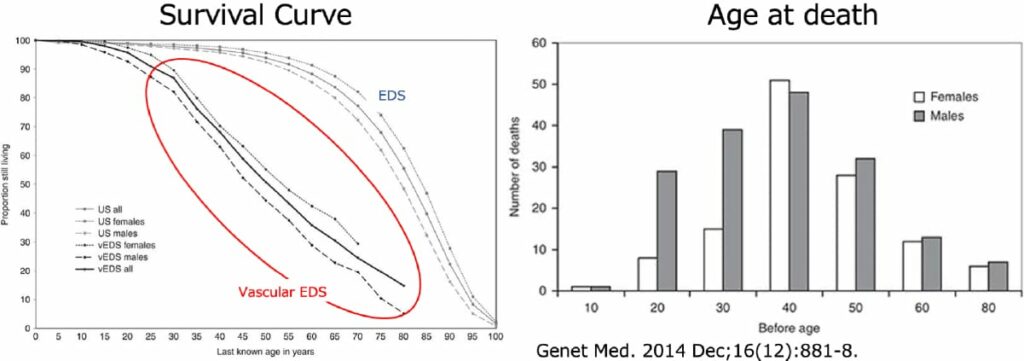
Please see Figure 2 below. A poor prognosis can be seen. The survival rate is 50% at the age of 50 years, and the number of deaths is highest among individuals in their 40 s.
What we medical professionals can do is to support the social life of patients as much as possible. Surgeons struggle to repair deteriorated tissues, but must also know the limits of surgery. Collaboration among departments is critical. Vascular surgeons operate the lesions directly, radiologists intervene on the lesions with endovascular techniques, colorectal surgeons and gynecologists operate gastrointestinal and uterine rupture, respectively, cardiologists and cardiovascular surgeons follow-up heart diseases, and psychologists provide mental support.
It is also important for patients to know the above-mentioned severe situation. Genetic consultation at the intractable disease information center in each facility, introduction of patient sites, etc. will also help.
