Treatments for peripheral ischemic arterial diseases
What symptoms occur because of blood flow obstruction in the legs?
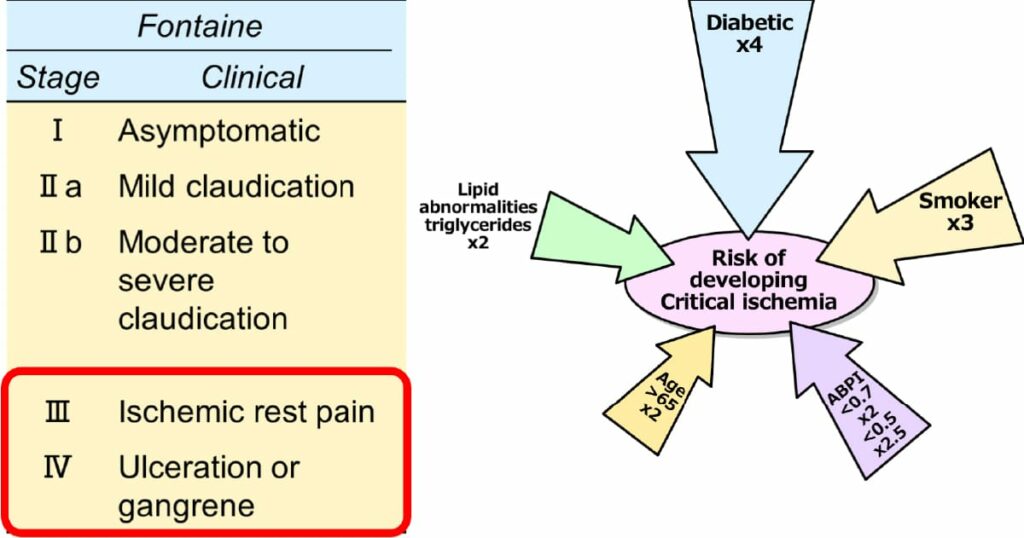
Blood flow obstruction in the leg is mainly caused by arteriosclerosis. Symptoms progress from a cold sensation, intermittent claudication (calf pain during exercise such as walking), rest pain (pain in the legs even at rest), to ulcer/necrosis. It becomes more severe according to the stage (Fig. 1, left). If obstruction or stenosis of the arteries due to arteriosclerosis causes ischemia, the worst-case scenario without treatment is amputation of the foot or death following sepsis. When ulcers or necrosis occur, the skin barrier is lost, making the tissues more susceptible to infection. Bacteria can easily enter the body and can be life-threatening if sepsis occurs. Diabetes and smoking are risk factors for developing critical limb ischemia (Fig. 1, right). The term Critical limb ischemia was previously used; however, chronic limb threatening ischemia (CLTI) is the commonly used technical term now.
Know your disease and know your treatment option. What about the prognosis?
The presence of arteriosclerotic lesions in the legs means that there may be other arteriosclerotic lesions in the body’s vasculature. In fact, about half of patients with ischemia in the leg have lesions in the coronary arteries, and a quarter have cerebrovascular atheromatous diseases (from the REACH registry). Therefore, the prognosis in this cohort of patients with leg ischemia is poor.
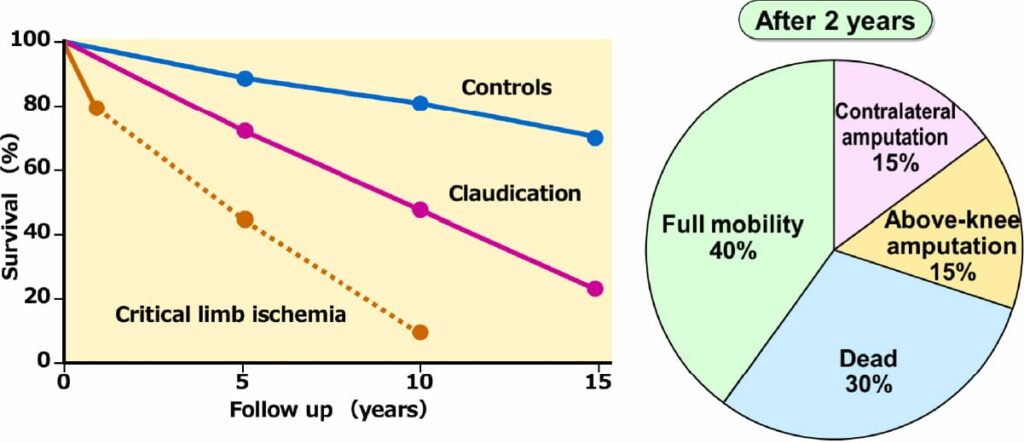
Figure 2. shows that the survival rate for patients with severe ischemia is 40% at 5 years (from the TASCII guidelines); It is much worse than that reported for advanced cancer of the stomach or colon. However, there are various causes of death such as myocardial infarction, cerebral infarction, sepsis, and pneumonia in patients with leg ischemia. They are invisible enemies, unlike cancer. “Unclear and invisible danger” causes a lack of awareness of the life-threatening crisis and delay in noticing the progress of ischemia.
In our department, we have operated a number of patients whose condition was thought to be difficult or impossible to manage with bypass surgery. Accumulation of successful bypasses resulted in a better survival rate compared to that shown in the graph (Fig. 2). We continue to contribute to improving the prognosis of patients with bypass, endovascular therapy, medication, and foot care.
What if you amputate a necrotic leg? the chart on the right in Figure 2 shows that in two years, 30% of the patients died. The reason may be that amputation caused further loss of activity, weakness, and vulnerabilities to infection. Therefore, we vascular surgeons are using bypass surgery as a weapon to “leave the foot, at least the heel”.
What is the treatment strategy?
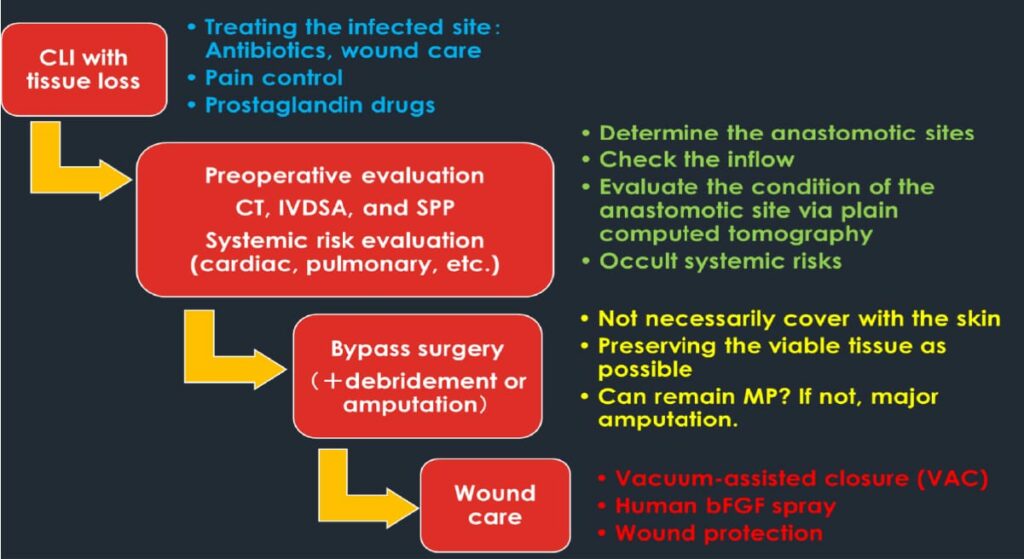
Most of the patients admitted to our department are in stages III and IV in Fig. 1. The treatment steps are shown in Fig. 3. Immediately after hospitalization, pain is relieved with analgesics, antibiotics are prescribed for controlling or preventing infection, and physiological and radiological examinations are performed to evaluate the condition of the patient in preparation for surgery.
In our department, the outcomes of bypass surgery have been excellent, with low mortality and high bypass patency rates compared to such data in Japan. The distal anastomosis method is popular among vascular surgeons as the “2 to 5 points suture method” and was introduced as a model technique during the bypass workshop sponsored by the academic society.
Recently, endovascular treatment has become popular, but the idea of ”expanding a stenotic lesion with a balloon or a stent because it’s there.” is extremely dangerous. Endovascular treatment may seem minimally invasive but may cause damage to the intima leading to re-stenosis or obstruction within a short period. For this reason, some patients receive treatment many times, eventually leading to amputation. When such patients come to our department, we frequently find devastated arteries that were healthy before endovascular procedures, and do not find appropriate target arteries for bypass surgery. Bypass has a high patency rate, and even if the artery is obstructed, the native arteries’ condition only returns to its original state, so we can take the next step in the treatment. In our opinion, bypass should be done first! Endovascular treatments should be used after careful discussion, considering the patients’ condition and pathology. Now that endovascular devices are evolving, we are pleased to possess more weapons. However, we must keep in mind that the weapons can also have a negative impact, depending on how they are used.
A case of severe ischemic foot
This is the case of an elderly woman with severe ischemic foot. She was told to undergo leg amputation to save her life at another hospital and was admitted to our hospital for a second opinion. It can be seen that the ischemic foot with necrosis has healed after surgery (Fig. 4). This patient is now enjoying her life, and carrying out activities such as playing golf and traveling. This is just one case, and not all cases work so well. What is important is awareness of the patient’s foot care, guidance by the vascular nurse, routine checkup by vascular surgeons, and management of the primary disease by specialists for diabetes, dialysis, and hyperlipidemia. All these factors can contribute to a better prognosis of the foot and life.

