Treatment for abdominal aortic aneurysm
What is an abdominal aortic aneurysm (AAA)?
The average diameter of the abdominal aorta is approximately 2 cm (2.5 cm in thoracic aorta). A dilated aorta > 3 cm (1.5 times the normal diameter) is called an “aneurysm” We regard 5.0 cm (2.5 times the normal aorta) aorta diameter as the threshold for indication for surgery and increased risk of rupture.
| Maximal minor diameter of abdominal aortic aneurysm (cm) | Risk of Rupture (%/year) |
|---|---|
| < 4 | 0 |
| 4 − 5 | 0.5 − 5 |
| 5 − 6 | 3 − 15 |
| 6 − 7 | 10 − 20 |
| 7 − 8 | 20 − 40 |
| > 8 | 30 − 50 |
(Figure 1)
Although AAAs rarely rupture in the 4-cm range, the annual rupture rate increases to 3%−15% when the diameter reaches 5 cm (Fig. 1).
In most cases, there are no symptoms. AAA is often found incidentally during health screening. Some patients come to the hospital with complaints such as “there is a lump pulsating in my stomach.”
What is the indication for surgery?
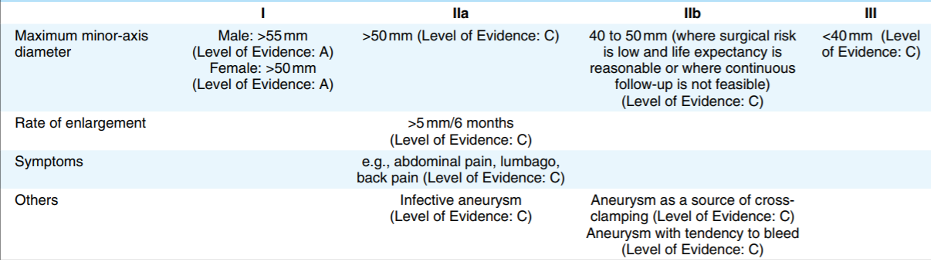
No matter how safe it may be, no one willingly opts for surgery. Mortality cannot be zero, and the actual complications are unknown. However, patients have to select surgical treatment because AAA may rupture. There is a guideline in Japan (Guidelines for Diagnosis and Treatment of Aortic Aneurysm and Aortic Dissection [JCS 2011]) (Fig. 2), which indicates the threshold AAA diameter. Generally, surgical treatment is definitely recommended for AAAs ≥ 55 mm, strongly recommended for AAAs ≥ 50 mm, and not actively recommended for AAAs < 50 mm.
How to operate?
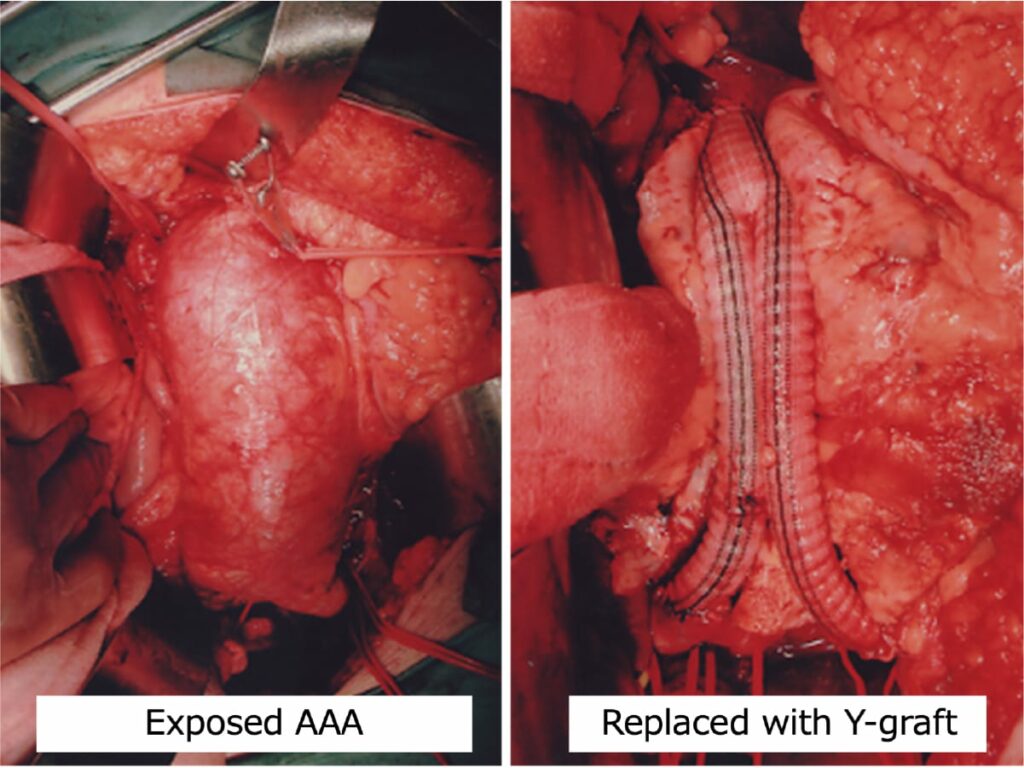
Surgical techniques include open surgery (aneurysm resection with graft replacement) (Fig. 3) and endovascular aneurysm repair (EVAR) with stent graft insertion (Fig. 4).
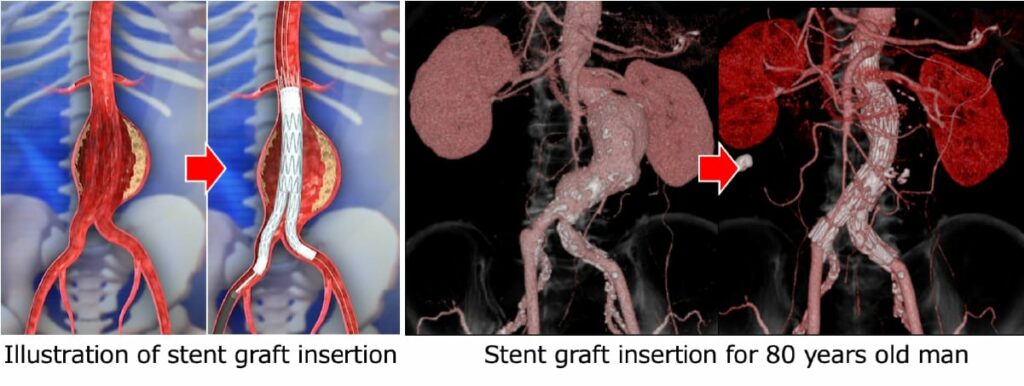
Which one is better? Stent graft treatment using a catheter or wire is regarded as a minimally invasive surgery with a small incision and short hospital stay. This “minimally invasive” treatment sounds good.
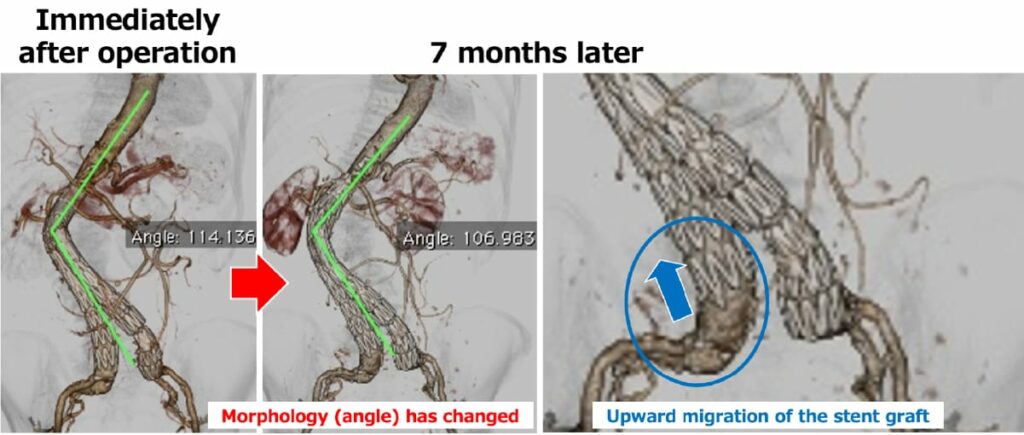
However, there are drawbacks of stent graft treatment. A stent graft is a technique that bridges the top and bottom of the aneurysm to prevent blood pressure from being exerted on the aneurysm wall. Unlike open surgery, where the artificial graft is directly sewn on the aortic tissue with sutures, the stent graft is anchored by a small hook or with friction forces due to oversized stent graft compared to the native aorta. After stent graft treatment, the remnant AAA sac is expected to shrink. However, some sacs annually increase in size. It is necessary to carefully check the stent graft for several years for migration or the emergence of leakage. If any adverse event is found, additional intervention is required. Therefore, we ask the patients to select “one big operation (open surgery) or several small ones (stent graft treatment).”
The average national in-hospital mortality rate of open surgery has been reported to be 2−3%. It is 1−2% in facilities that perform a high-number of surgeries (high volume center). Fortunately, in-hospital mortality is as low as 0.2% in our department, and there have been no in-hospital deaths for the past 20 years. We assume that various tests unique to university hospitals and the close collaboration with other departments (cardiology, anesthesiology, ICU staff, etc.) may prevent serious surgical complications.
Risks of stent graft treatment
Patients with risk factors mentioned in Figure 5 are eligible for stent grafting.
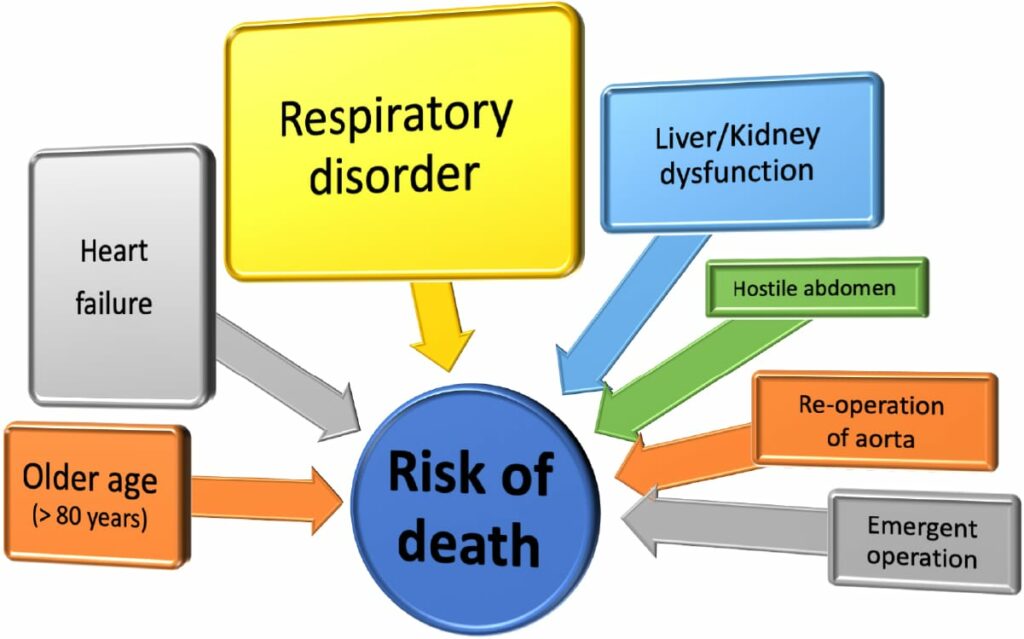
Open surgery is recommended for patients who do not have these factors. The guidelines of the Ministry of Health, Labor, and Welfare also state that the first-line therapy for AAA should be open surgery. We have used stent grafts since they were introduced in Japan and have recognized that EVAR is not necessarily safe and durable due to stent graft migration, late-phase leakage, device failure, and late AAA sac enlargement. We have sounded the alarm on selecting EVAR without considering the patients’ background or AAA anatomy (Fig. 6).
In 2017, the report of outcomes of EVAR performed in Japan (analysis of 38,008 AAA cases) was published. (Hoshina, et al. Ann Surg 2017) It demonstrated the risk factors mentioned above and real-world data of outcomes such as mortality rate and complication rate. The most surprising data was the AAA sac enlargement (≥5 mm) was found in 23% of cases 5 years after EVAR (Fig. 7).
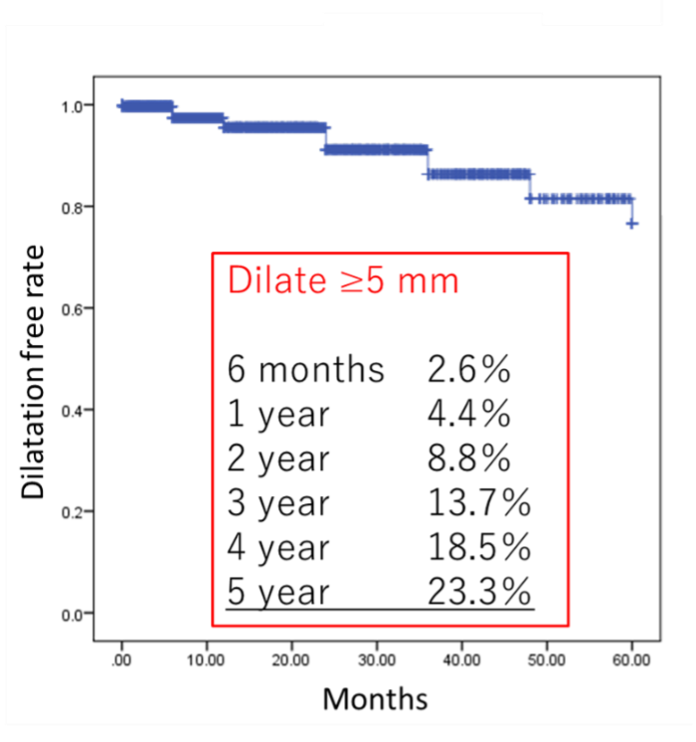
If the aneurysm grows, we should consider some additional intervention. Some facilities have selected EVAR rather than open surgery without considering patients’ long-term prognosis, backgrounds, and anatomy because it is minimally invasive and profitable, there are a large number of cases with sac enlargement several years after EVAR. They have to pay the price for it now (have to do re-intervention). Such unexpected matters had been repeated many times in the medical history, every time new devices emerged. Now that an excellent treatment method – EVAR – emerged, we must use it appropriately and improve it to a more complete one. To that end, we consider each patients’ long-term prognosis, backgrounds, and anatomy and determine the indication with careful discussion. There are many examples of what is now correct but turns out to be wrong 10 years later. We surgeons must keep collecting data and keep thinking so that patients can have better outcomes in the future.
What type of stent graft is best suitable for me?
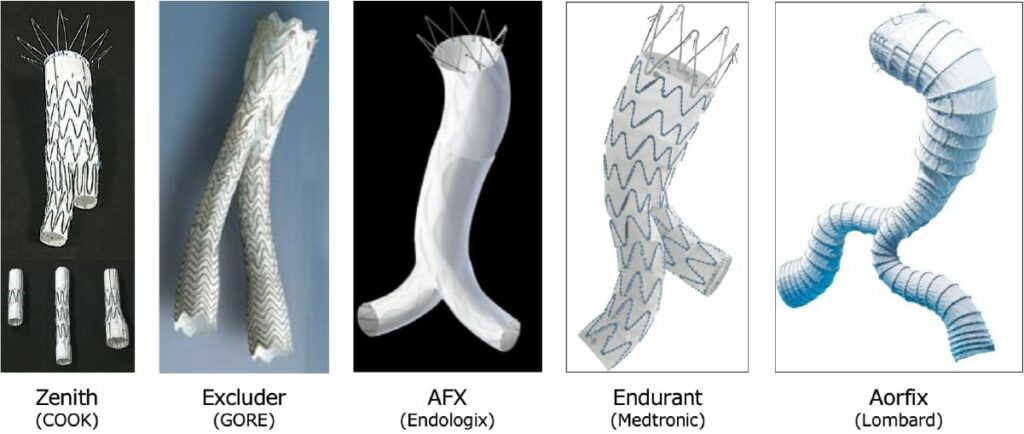
There are several stent grafts currently on the market and each has its own characteristics (Fig. 8). Any device can be used as long as it meets the anatomical instructions for use. At the beginning of the EVAR introduction, the operators preferred to select the device what they got used to using or the device whose procedure steps were simpler and easier to understand. However, as the operators accumulated the experiences, devices which are more suitable for patients’ anatomy came to be selected. In our conference (grand rounds), the doctors in charge have to present the reason (i.e. angulation, short neck, narrow terminal aorta and patients’ prognosis) why they select the device. Therefore, if you ask our staff the reason of selecting the device, they can answer to it. By conducting such detailed preoperative evaluations, we believe that the stent graft treatment will improve the perfection and we can demonstrate the excellent long-term outcomes equal to open surgery in the near future.
(* Although it has not been published, the above-mentioned Japanese registry data shows results for each device, and there are differences of outcomes among devices.